Tuberculosis of the Spine
Tuberculosis (TB) is a chronic granulomatous infection caused by Mycobacterium Tuberculi. Tuberculosis of the Spine is also called Pott's disease and accounts for 2-5 percent of all TB cases.
TB spine can be divided into early and late infections. Treatment depends on the stage of presentation.
Early Spinal TB - early in the disease the vertebral bodies are affected by the infection. Following this paraspinal abscesses can form which present as large collections. TB characteristically doesnt involve disc spaces and can sometimes be confused with cancer on standard spinal imaging.
Late or Chronic Spinal TB - Late infections typically present as pain related to spinal deformities such as kyphosis. This occurs due to destruction and collapse of the vertebral bodies. Deformities are more severe if the infection occurs in younger children and can progress with growth of the spine. In adults usually the deformity is static.
CLINICAL SYMPTOMS
- The onset of symptoms is characteristically very slow and long drawn in TB.
- Typically patients have malaise, fatigue, night sweats, anorexia and weight loss.
- Back pain is usually a late symptom and is related to the extent of bony destruction and deformity leading to spinal instability or arthritis.
- Patients may notice that they are more forward bent (kyphotic) than before. They may notice a bony prominence over the spine (gibbus). Patients may notice weakness in their legs and loss of balance. Very rarely they may lose control over bowels or bladder function.
INVESTIGATIONS
BLOOD TESTS - Blood counts can show increased lypmphocytes. Inflammatory markers such as CRP and ESR can be elevated. Tuberculin PPD can be elevated in 80 percent cases.
SPINAL RADIOLOGICAL IMAGING-
- Chest X ray - 65 percent of patients with spinal TB will have an abnormal chest Xray.
- MRI with Gadolinium contrast - MRI remains the diagnostic imaging of choice for spinal TB. It is highly sensitive and specific to diagnose spinal TB and also requires an expert radiologist to recognise the classical radiological patterns.
- CT scans - can be used to better delineate the extent of bony destruction and epidural spread of the disease.
- Nuclear Medical Scans - these are highly sensitive to detect TB spine
INVASIVE SPINAL INVESTIGATIONS
CT guided spinal biopsy - CT guided biposy performed under local naesthetic byt the radiologist confirms the diagnosis of TB after Acid Fast Bacillus positive staining of the specimens
Open Surgical Biopsy - In some cases an open surgical biopsy under General anaesthetic is undertaken by the surgeon if the area is difficult to access on CT or if there is a failed CT biopsy.
TREATMENT
PHARMACOLOGICAL TREATMENT-
TB has become a medical disease in the recent years. The treatment of early stage infection remains pharmacological. Rifampicin, Isoniazid, Pyrazinamide and Ethambutol for two months followed by Rifampicin and Isoniazid for 9-18 months depending on response to treatment and blood test results. Treatment of drug resistant TB can be different.
SURGICAL TREATMENT -
Indications of surgical treatment are very specific -
- Acute severe paralysis
- Progressing neurological deficit despite medical treatment
- Late spinal instability and kyphosis with or without progressive neurological deficit
- Progressive kyphosis despite treatment
- Large severe caseation and abscesses which are inaccessible to antibiotic and amenable to radiological drainage
- failure of nonoperative treatment after 3 to 6 months
- diagnosis uncertain
Deformity Surgeries are complicated and involve anterior surgery combined with anterior - posterior instrumentation. The risks of paralysis are higher in these cases especially if there is pre-exisiting neurological deficit and a diseased spinal cord as a result of chronic compression.
Figure 1 - Chronic TB with Thoraco Lumbar Kyphosis and severe destruction of the vertebral body.
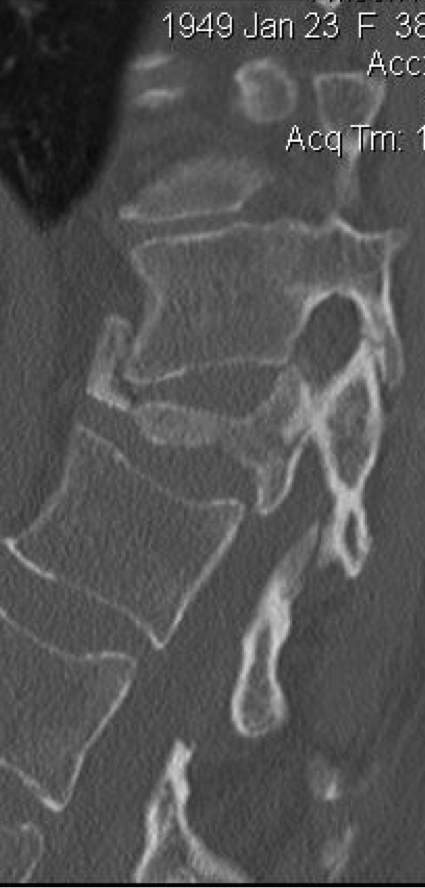
Figure 2 - Post-Op Xray in Chronic TB showing anterior corpectomy and correction of kyphosis with posterior and anterior instrumentation

